-
About Usin etymology
-
Accident and Emergencyin Specialities
-
Ambulance Servicesin facilities
-
Anaesthesiologyin Specialities
-
Blood Bankin facilities
-
Cardio Thoracic Surgeryin Specialities
-
Cardiologyin Specialities
-
Cardiothoracic Intensive Care Unitin facilities
-
Careersin etymology
-
Catheterization Laboratoryin facilities
-
Child Development Centerin facilities
-
Clinical Laboratoryin facilities
-
Clinical Psychologyin facilities
-
Day Care Service Suitein facilities
-
Dentistryin Specialities
-
Dermatologyin Specialities
-
Diabetologyin Specialities
-
Dialysisin facilities
-
Dr S Hemanthin doctors
-
Dr. Adithya Venkataramanan Ain doctors
-
Dr. Vignesh Sankarin doctors
-
Dr.ADARSH SURENDRANATHin doctors
-
Dr.ADHAVAN Ein doctors
-
Dr.Akshaya Keerthikhain doctors
-
Dr.Anirban Lahain doctors
-
Dr.Anisha Kumari.A.Jin doctors
-
Dr.ANITHA.Rin doctors
-
Dr.Antony Leo Jerry.Tin doctors
-
Dr.Anu Suganya.J.Bin doctors
-
Dr.AQIB.Min doctors
-
Dr.ARATHI SURENDRANATHin doctors
-
Dr.Arulmozhiin doctors
-
Dr.Arulmurugan Din doctors
-
Dr.Arun Prasad Din doctors
-
Dr.ARUN RAMANANin doctors
-
Dr.ARUNA RANI.P.Kin doctors
-
Dr.Arvindh Raj.B.Kin doctors
-
Dr.Arvindraj Rin doctors
-
Dr.ASHOKKUMARin doctors
-
Dr.Aswin Gin doctors
-
DR.AVINASH R.Min doctors
-
Dr.BALARAMAN Rin doctors
-
Dr.BASKAR. Ain doctors
-
Dr.BHAIRAVI T.Gin doctors
-
Dr.Bharath.Nin doctors
-
Dr.BINO JOHN SAHAYO Jin doctors
-
Dr.Brinda Kin doctors
-
Dr.C.R.Lakshmi Narayananin doctors
-
Dr.Chandan Y Sin doctors
-
Dr.CHELLAPANDIANin doctors
-
Dr.CHITRA PADMANABHANin doctors
-
Dr.DEEPAK KUMAR K.Sin doctors
-
Dr.Deepak Kumar Selvanathanin doctors
-
Dr.DEEPAK P Sin doctors
-
Dr.DEEPARANI.Vin doctors
-
Dr.DEVACHANDRAN.Jin doctors
-
Dr.DEVI Cin doctors
-
Dr.Dinesh Pin doctors
-
Dr.divya.Din doctors
-
Dr.EDIN BROW Din doctors
-
Dr.GEETHALAKSHMIin doctors
-
Dr.Ghurulakshmi Moorthyin doctors
-
Dr.Gopinath Venkatesanin doctors
-
Dr.Harapriya.Bin doctors
-
Dr.HEMALATHA Pin doctors
-
Dr.Jagannath Soundarajanin doctors
-
Dr.JAIKUMAR.Vin doctors
-
Dr.Janani Arulin doctors
-
Dr.JAYANTHI GOVINDRAJANin doctors
-
Dr.JAYARAJ.A.Kin doctors
-
Dr.JEEVITHA Rin doctors
-
Dr.JOSEPH DOMINICin doctors
-
Dr.K.JAYACHANDRANin doctors
-
Dr.K.V.S.Lathain doctors
-
Dr.KALA.Kin doctors
-
Dr.KALAIYARASAN.Tin doctors
-
Dr.KALEEL RAHUMAN.M.Pin doctors
-
Dr.KARTHICK SRINIVASin doctors
-
Dr.KARTHIK SURYA.Rin doctors
-
Dr.KARTHIKEYAN DAMODHARANin doctors
-
Dr.KARTHIKEYAN PERUMALin doctors
-
Dr.KATHIRESAN.Nin doctors
-
Dr.Keerthana Balasubramanianin doctors
-
Dr.Keerthivasanin doctors
-
Dr.KIRUTHIKA RANGANATHANin doctors
-
Dr.Kishore.Din doctors
-
Dr.KRISHNA KUMAR.Pin doctors
-
Dr.KUMAR SAMPATHin doctors
-
Dr.KUMARAN GNANASEKARANin doctors
-
Dr.KUMARAVEL.Gin doctors
-
Dr.M.M.SHANKARin doctors
-
Dr.MADHUBALA Kin doctors
-
Dr.Madhumita Cin doctors
-
Dr.MAJOR G VASANTH KUMAR (Retd)in doctors
-
Dr.MANIKANDAN Kin doctors
-
Dr.MEERA RANI NAYAKin doctors
-
Dr.MOORTHY Gin doctors
-
Dr.Mridulla Abiramiin doctors
-
Dr.N.MAHESHin doctors
-
Dr.NAGALEKSHMI.Gin doctors
-
Dr.NANDINI GOVINDARAJANin doctors
-
Dr.Naresh Kumar Sin doctors
-
Dr.NAVEENin doctors
-
Dr.NITHYAKALYANIin doctors
-
Dr.P NIRMALA DEVIin doctors
-
Dr.PARTHIBANRAJ RAGUNATHANin doctors
-
Dr.PILLAI C.Vin doctors
-
Dr.PILLI ALEKHYAin doctors
-
Dr.PORKODIin doctors
-
Dr.PRAHADA.Jin doctors
-
Dr.PRASANNA VENKATESH KANDASAMYin doctors
-
Dr.Praveen Chander Nin doctors
-
Dr.PREM SEKAR.Rin doctors
-
Dr.PRIYA Bin doctors
-
Dr.Priyanka M Vin doctors
-
Dr.R VIDYACHAYAin doctors
-
Dr.RAJAPRABU.Tin doctors
-
Dr.RAJESHWARI Nin doctors
-
Dr.RAJESWARI RAMACHANDRANin doctors
-
Dr.Rajkumar Iin doctors
-
Dr.RAJKUMAR Pin doctors
-
Dr.RAJKUMAR RATHINASAMYin doctors
-
Dr.RAJKUMAR Sin doctors
-
Dr.Rameez Raja Bin doctors
-
Dr.Ramkumarin doctors
-
Dr.RAMYAin doctors
-
Dr.RAMYA.Rin doctors
-
Dr.REJIVin doctors
-
Dr.ROHINI Iin doctors
-
Dr.ROSY ELANCHEZHIANin doctors
-
Dr.S Arun Victor Jebasinghin doctors
-
Dr.S.S.K.SANDEEPin doctors
-
Dr.S.Shruthi Shreein doctors
-
Dr.Sai Surendarin doctors
-
Dr.Saketh Ramineniin doctors
-
Dr.Sakthivelin doctors
-
Dr.SAMUEL EBENEZER.Fin doctors
-
Dr.Santhosh Min doctors
-
Dr.SANTHYA.T.Vin doctors
-
Dr.SARAVANNAN.Jin doctors
-
Dr.SARAVANNAN.Sin doctors
-
Dr.SASIKALA Min doctors
-
Dr.SAVITHA.Ain doctors
-
Dr.SELVAKUMAR.Cin doctors
-
Dr.Selvapandiyan Paulin doctors
-
Dr.SENTHILKUMAR.Din doctors
-
Dr.Shashidhar.R.Ain doctors
-
Dr.Sivakumar Ganesanin doctors
-
Dr.SIVARANJINI.T.Gin doctors
-
Dr.Sowmya Sin doctors
-
Dr.Sreekaanth.Sin doctors
-
Dr.Sreelakshmiin doctors
-
Dr.SUBALAKSHMI Hin doctors
-
Dr.SUCHITRA RAVISHANKARin doctors
-
Dr.sujaya Raghavendrain doctors
-
DR.SUMANA PREMKUMARin doctors
-
Dr.SUMATHY.Vin doctors
-
Dr.SURENDRAN.Jin doctors
-
Dr.Suriyakanthin doctors
-
Dr.SWAMINATHAN.T.Sin doctors
-
Dr.Swathy Prasannain doctors
-
Dr.THAYAPARAN Sin doctors
-
Dr.THILAKH BABU. Rin doctors
-
Dr.THIRUMALAI.Pin doctors
-
Dr.USHA.Sin doctors
-
Dr.VAIDEESWARAN Min doctors
-
Dr.VIDHYA MOHANDOSSin doctors
-
Dr.VIDYA.Rin doctors
-
Dr.Vignesh Gokul Venkatachalamin doctors
-
Dr.VIJAYAKARTHIKEYANin doctors
-
Dr.Vijayanidhi Karunanidhiin doctors
-
Dr.VINOTH KUMAR A.Vin doctors
-
Dr.Vivek Sin doctors
-
Dr.VIVEKANAND Pin doctors
-
Dr.YASHWANT SUNDARin doctors
-
Endocrinologyin Specialities
-
ENT Ear Nose Throatin Specialities
-
Eventsin medium
-
Executive Boardin etymology
-
Family Medicinein Specialities
-
Fertility Centrein facilities
-
Fertility Medicinein Specialities
-
Gastroenterologyin Specialities
-
General Medicinein Specialities
-
General Surgeryin Specialities
-
Geriatricsin Specialities
-
Hepatologyin Specialities
-
Imaging Servicesin facilities
-
Institute of Medical Science and Researchin etymology
-
Insurance / Tie-upsin facilities
-
Intensive Care Unit-ICUin facilities
-
IVF Treatmentin Specialities
-
Labour Wardin facilities
-
Lactationin Specialities
-
Medavakkamin location
-
Media Articlesin medium
-
Medical Oncologyin Specialities
-
Milestonesin etymology
-
Mrs.Anitha Mary Oyasisin doctors
-
Mrs.VIJAYALAKSHMIin doctors
-
Ms.Akshaya Karthikeyanin doctors
-
Ms.Krishna Priya Pin doctors
-
Neonatal Intensive Care Unit-NICUin facilities
-
Neonatologyin Specialities
-
Nephrologyin Specialities
-
Neuro Laboratoryin facilities
-
Neuro Surgery and Trauma Carein Specialities
-
Neurologyin Specialities
-
Newsletterin medium
-
Obstetrics and Gynaecologyin Specialities
-
Occupational Therapyin facilities
-
Oncologyin Specialities
-
Operation Suitein facilities
-
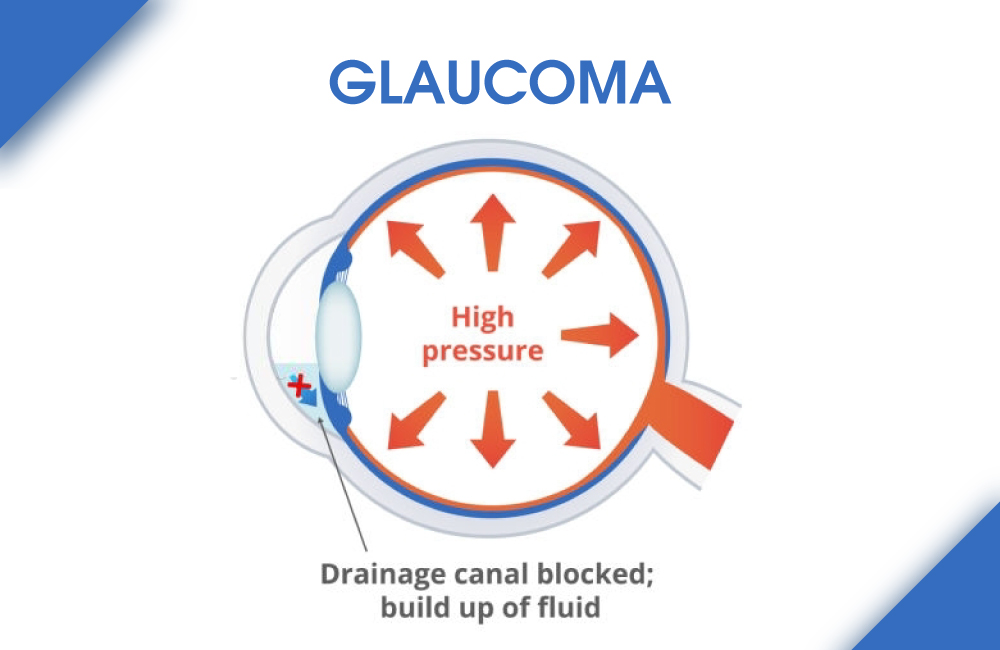
Ophthalmologyin Specialities
-
Orthopaedicsin Specialities
-
Out Patient Consultants Suitein facilities
-
Paediatric Cardio Thoracic Surgeryin Specialities
-
Paediatric Cardiologyin Specialities
-
Paediatric Endocrinologyin Specialities
-
Paediatric Neurologyin Specialities
-
Paediatric Physiotherapyin Specialities
-
Paediatric Psychiatryin Specialities
-
Paediatricsin Specialities
-
Pain Managementin Specialities
-
Patient Room Suitein facilities
-
Pediatric Intensive Care Unit-PICUin facilities
-
Pharmacyin facilities
-
Physiotherapyin facilities
-
Plastic and Cosmetic Surgeryin Specialities
-
Press Releasein medium
-
Preventive Health Carein facilities
-
Psychiatryin Specialities
-
Pulmonologyin Specialities
-
Radiation Oncologyin Specialities
-
Radiologyin Specialities
-
Rheumatologyin Specialities
-
Scopy Suitein facilities
-
siruseriin location
-
Social Postsin medium
-
Speech Therapyin facilities
-
Surgical Gastroenterologyin Specialities
-
Surgical Oncologyin Specialities
-
Transplant ICUin facilities
-
Transplant Surgeryin Specialities
-
Urologyin Specialities
-
Vascular and Endovascular Surgeryin Specialities
-
Videosin medium
-
Vision & Missionin etymology